Minor cuts, scratches, and blisters are normal side effects of an active life. If your body’s wound-healing processes function properly, you may not even notice such small injuries, because they heal so quickly.
However, that’s not the case for people with diabetes. If you’re living with diabetes, you probably know that even insignificant scrapes and sores can intensify into dangerous wounds.
By understanding exactly why diabetic wounds take longer to heal and learning more about the best diabetic wound care treatment options available, you can be sure to avoid the dangerous complications of diabetic wounds and maintain a strong quality of life.
What Makes Diabetic Wounds Different From Regular Wounds?
What makes diabetic wounds so different from regular wounds? It’s an important question to explore so that you can receive the diabetic wound care you need to protect your body from serious complications.
The Body’s Normal Wound-Healing Process
A wound is considered a break or opening in the skin. Since your skin protects the rest of your body from pathogens and bacteria, it’s easy for a wound like a puncture or cut to cause infection.
In a body unaffected by diabetes, every wound triggers a natural healing process that begins within minutes of the injury. Blood flows and eventually clots to form a scab, which serves the valuable purpose of protecting underlying tissues from bacteria.
Once the scab has formed, the immune system fights off infection by opening nearby blood vessels to deliver oxygen and nutrients to the wound. This makes it possible for powerful white blood cells to prevent infection, combat germs, and support the wound as it heals.
This entire process usually only takes about two to five days, but invisible healing continues for weeks as the body repairs broken blood vessels and grows new tissue.
The Healing Process With Diabetes
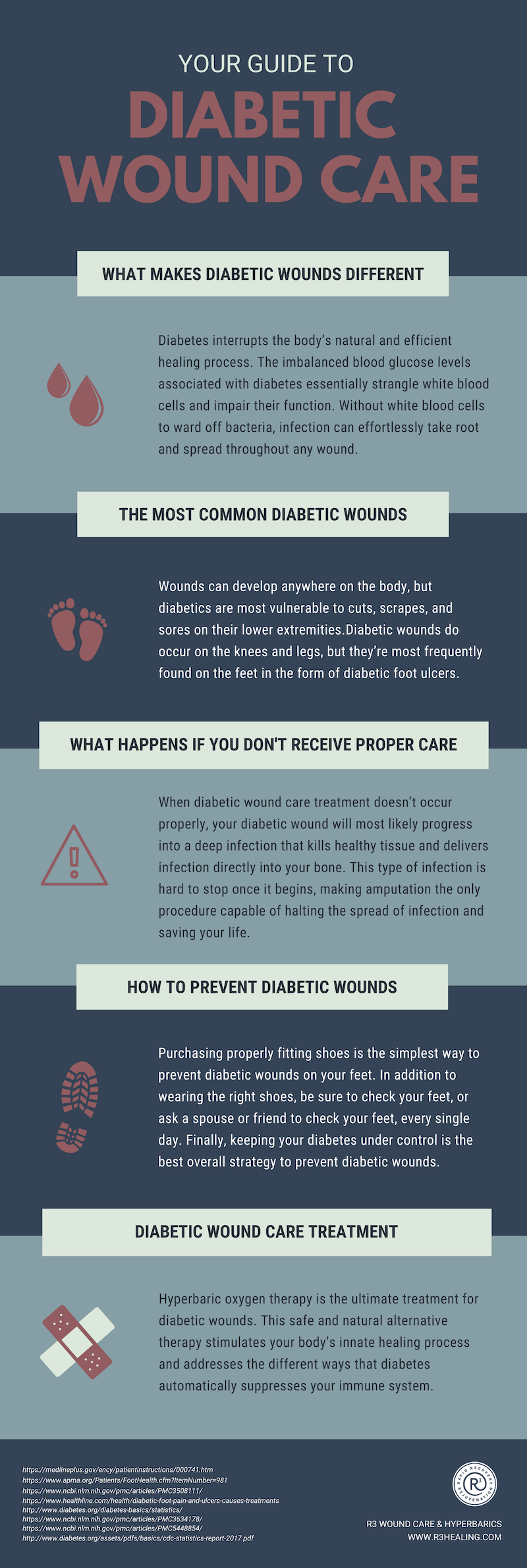
Unfortunately, diabetes interrupts the body’s natural and efficient healing process. The imbalanced blood glucose levels associated with diabetes essentially strangle white blood cells and impair their function. Without white blood cells to ward off bacteria, infection can effortlessly take root and spread throughout any wound.
Diabetes is also associated with poor circulation, which further compounds the problem, because strong circulation is needed for red blood cells to deliver nutrients to the wound. This leaves the wound vulnerable to infection and deficient in the nutrients it needs to heal.
Worse yet, diabetes also causes nerve damage. This means that you might not be able to feel or sense the infected, slow-healing wound on your body. In fact, of the 15 percent of diabetic patients who suffer from diabetic foot ulcers, nearly half are hospitalized due to severe complications, and nearly 25% must undergo amputation.
This explains why diabetes is the leading cause of non-traumatic lower extremity amputation in the United States! Diabetes severely restricts the body’s natural healing mechanisms and creates the perfect conditions for infection to develop.
Share this Image On Your Site
The Most Common Diabetic Wounds
Wounds can develop anywhere on the body, but diabetics are most vulnerable to cuts, scrapes, and sores on their lower extremities.
Diabetic wounds do occur on the knees and legs, but they’re most frequently found on the feet in the form of diabetic foot ulcers. Given that diabetic foot problems are the most common cause of hospitalization among diabetic patients, proper treatment is essential to long-term health.
What Is a Diabetic Foot Ulcer?
A diabetic foot ulcer begins just like any normal wound. It might be a cut, scrape, blister, or other minor injury. The complications of poorly controlled diabetes, including slow circulation and nerve damage, prevent such wounds from healing normally. Instead, the skin breaks down further and exposes deeper layers of tissue to bacteria and infection.
Do You Have a Diabetic Foot Ulcer?
Since nerve damage may prevent you from feeling the pain of your diabetic foot ulcer, it’s important to visually inspect your feet every day. If you notice any of the following signs, seek medical care immediately:
- Drainage from your foot is staining your socks or leaking from your shoe
- Unusual swelling
- Irritation and redness
- Strong, irregular odor from one or both feet
- Black tissue surrounding a wound on the foot
Many diabetic foot ulcers develop under the big toe and along the balls of the feet. The earlier you can identify your diabetic foot ulcer and receive treatment, the better your chances of preventing severe complications.
What Happens If Your Diabetic Wound Doesn’t Receive Proper Care?
Unfortunately, your diabetic wound won’t simply disappear if you ignore it. Instead, a wound like a diabetic foot ulcer will become more and more severe until it threatens your entire foot or even your life. In fact, diabetic foot ulcers precede about 85% of all amputations performed on adults with diabetes!
When diabetic wound care treatment doesn’t occur properly, your diabetic wound will most likely progress into a deep infection that kills healthy tissue and delivers infection directly into your bone. This type of infection is hard to stop once it begins, making amputation the only procedure capable of halting the spread of infection and saving your life.
This is why the most common diabetic amputations occur on the toes, feet, and lower legs. More than 70,000 Americans endure amputations due to diabetic complications every year, but they’re largely preventable with proper diabetic wound care and attention.
What’s the Connection Between Blood Sugar Levels and Wound Care?
Nearly 10% of the U.S. population has diabetes, which means that more than 30 million people struggle to maintain balanced blood sugar levels on a regular basis.
Diabetes develops when your body cannot properly produce or use insulin, the hormone that transforms sugar into usable energy. When insulin can’t do its job, glucose builds up in the blood and causes severe health complications.
High blood sugar stifles your body’s natural healing functions in a few critical ways:
- Triggers inflammation throughout the body
- Weakens the immune system’s protections
- Blocks nutrients and oxygen from strengthening and energizing injured cells
- Prevents white and red blood cells from traveling to wound
Inefficient healing mechanisms don’t stand a chance against out-of-control infection. This is especially true since bacteria thrive on the excess sugar available in the bloodstream of a person with diabetes. Weak healing functions, rapidly reproducing bacteria, and untreated infection create the perfect storm for severe, non-healing diabetic wounds.
How to Prevent Diabetic Wounds
The risks associated with diabetic wounds are frightening, but it’s possible to prevent them altogether! Take the following precautions to minimize your likelihood of developing a non-healing diabetic wound.
Check Proper Shoe Fit
Purchasing properly fitting shoes is the simplest way to prevent diabetic wounds on your feet. Ill-fitting shoes rub and cause blisters to form, and those blisters quickly lead to diabetic foot ulcers. The right shoes will be tight enough to stop fabric from rubbing against the skin, but loose enough to fit all toes comfortably. Many diabetic patients even choose specialty orthopedic shoes that are custom made to fit the size, shape, and contours of their feet.
Check and Wash Your Feet Daily
In addition to wearing the right shoes, be sure to check your feet, or ask a spouse or friend to check your feet, every single day. Diabetic nerve damage makes it much harder for you to feel any pain caused by wounds, so only a visual inspection will reveal signs of injury. Look carefully for cuts, cracks, and blisters. Check closely around the nails since this area is especially vulnerable to infection.
Also make sure to wash your feet at least once a day with warm water and dry them afterwards. It’s important to dry between each individual toe so that moisture doesn’t accumulate and breed bacteria. Take this time to gently trim your toenails in a way that prevents ingrown nails. Moisturize your feet after washing to minimize cracking and chafing as well.
Control Your Blood Sugar
Of course, keeping your diabetes under control is the best overall strategy to prevent diabetic wounds. Working with your doctor to treat your diabetes with diet, exercise, and medication adjustments can have a huge influence on the efficiency of your body’s natural wound-healing process and immune system.
If you can optimize the activity of red blood cells, white blood cells, and your overall circulatory system, you’ll begin to improve your body’s wound healing response and protect yourself from non-healing diabetic wounds.
Tips to Avoid Infection in Your Diabetic Wound
If you already have a diabetic wound, preventative measures are still important to stop future injuries, but they won’t be enough to avoid infection in your existing wound. The following tips will help you maximize the results of your diabetic wound care and prevent any infection-related complications.
Practice Proper Wound Care
You can’t ignore your diabetic wound and expect it to heal on its own. The very fact that you have diabetes automatically makes wound healing more difficult. By practicing proper diabetic wound care, you will protect your wound from infection and help the healing process continue.
Proper wound care is different for every patient. The size, age, and condition of your wound determine the specific type of care you need to accelerate healing. A few possible wound care options include collagen skin substitutes, foam dressing, calcium alginates, and enzyme applications.
Avoid Sources of Infection
It’s also important to avoid major potential sources of infection, especially public swimming pools and hot tubs. These areas are breeding grounds for bacteria that effortlessly find their way into diabetic wounds and wreak havoc. Even soaking in the bathtub can give bacteria the opportunity to create an infection, so do your best to keep your shoes on and your feet dry.
Diabetic Wound Care Treatment Options
Whether your wound is already infected or you want to take extra precautions to prevent infection, the following diabetic wound treatment options can effectively accelerate your body’s healing response.
Diabetic Shoes and Boots
Your doctor may recommend Unna Boots or other diabetic shoes or boots to treat your diabetic wound. Unna Boots are compression bandages designed to provide a semi-solid mold around the foot and lower leg. The boots apply gentle pressure, but still allow movement, and the medicated paste on the inside of the boots keeps your diabetic wound moist to promote healing and provide protection against infection.
Hyperbaric Wound Care
Hyperbaric oxygen therapy (HBOT) is the ultimate treatment for diabetic wounds. This safe and natural alternative therapy uses the power of pressurized oxygen to stimulate your body’s innate healing process and address the different ways that diabetes automatically suppresses your immune system.
During an HBOT treatment, you lay comfortably in a special hyperbaric chamber and simply inhale concentrated oxygen. As this oxygen flows through your body, it dissolves directly into all of your body’s fluids and permeates areas where circulation is reduced or blocked.
How Does Hyperbaric Wound Care Help Your Diabetic Wounds Heal Faster?
Oxygen can only make its way through the blood within red blood cells. Since the circulation problems associated with diabetes slow the movement of red blood cells, important tissues become deprived of oxygen.
Without enough oxygen, cells struggle to produce the energy they need to block bacteria, synthesize new collagen, or regenerate and repair after injury. This is why diabetic wound healing slows until it comes to a full stop.
Inhaling the concentrated flow of oxygen provided through regular HBOT treatments makes it possible to overcome oxygen deficiencies and stimulate a more effective healing process.
By stimulating and supporting the body’s natural healing capabilities, HBOT helps your diabetic wounds heal faster. White blood cells finally get the oxygen they need to effectively kill bacteria, reduce swelling, and allow the rapid reproduction of new blood vessels. HBOT even helps cells build new connective tissue and improve organ function.
The team at R3 Wound Care and Hyperbarics offers state-of-the-art HBOT treatments designed to address your unique medical needs and help you enjoy your life without the hindrance and dangers of diabetic wounds. Our team can give you the treatment you need—no doctor referral is needed.
Learn more now to find out exactly why diabetic wound care with HBOT is the treatment that can change your life.
Resources:
1. How Wounds Heal. Medline Plus. https://medlineplus.gov/ency/patientinstructions/000741.htm
2. Diabetic Wound Care. APMA. https://www.apma.org/Patients/FootHealth.cfm?ItemNumber=981
3. Ingrid Kruse, DPM and Steven Edelman, MD. Clinical Diabetes 2006 Apr; 24(2): 91-93.https://doi.org/10.2337/diaclin.24.2.91
4. Diabetic Foot Pain and Ulcers: Causes and Treatment. Healthline. https://www.healthline.com/health/diabetic-foot-pain-and-ulcers-causes-treatments#causes
5. Alexiadou, K., & Doupis, J. (2012). Management of Diabetic Foot Ulcers. Diabetes Therapy: Research, Treatment and Education of Diabetes and Related Disorders, 3(1),4. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3508111/
6. Statistics About Diabetes. American Diabetes Association. https://www.diabetes.org/diabetes-basics/statistics/
7. National Diabetes Statistics Report, 2017. https://www.cdc.gov/diabetes/data/statistics-report/index.html
8. Iraj, B., Khorvash, F., Ebneshahidi, A., & Askari, G. (2013). Prevention of Diabetic Foot Ulcer. International Journal of Preventive Medicine, 4(3), 373-6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3634178/
9. Health Quality Ontario (2017). Hyperbaric Oxygen Therapy for the Treatment of Diabetic Foot Ulcers: A Health Technology Assessment. Ontario Health Technology Assessment Series, 17(5), 1-142. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5448854/
