Chrystal Changa,a *, Christine White a, Alan Katz b, Moneer K. Hanna c
Introduction Repeated and multiple surgeries for hypospadias result in varying degrees of scarring and hypo-vascularity of penile tissues which may result in poor healing and increasing complication rates with each additional repair. Vasodilator agents such as Nitroglycerine (NTG) can be helpful in the immediate postoperative period to improve flap viability. Hyperbaric oxygen therapy (HBOT) has well-established benefits in promoting angiogenesis and wound healing. We hypothesized that NTG and HBOT, methods to promote blood flow and wound healing, would provide better outcomes in redo hypospadias surgeries and reduce complication rates; and, that HBOT and NTG would provide better outcomes compared to NTG alone.
Herein, the authors review the results of their strategy of the past 5.5 years in managing these compromised hypovascular tissues using 2% NTG and HBOT for redo surgery of hypospadias.
Between 2014 and 2019, 82 patients (2e24 years old) exhibiting varying degrees of scarring of the skin and subcutaneous tissues underwent re-operative repair of hypospadias complications following failed surgeries (3e9 operations, average 5.5 failed previous repairs). There were two groups of patients: Group I (49 patients) received trimodal therapy consisting of NTG, HBOT, and local steroids. The patients were examined every 3 weeks and every 3 months thereafter. The postoperative site was photographed by the parents or by the older patient prior to each visit. Group II (33 patients) received NTG and local steroids, but not HBOT for various reasons.
In Group I: 44/49 (88.8%) of the repairs were successful. The complications in this group included a distal repair breakdown (n Z 2) and a urethral fistula (n Z 3). In Group II, a successful outcome was noted in 23/33 (69.6%). The follow-up of the 78 patients who completed their repairs varied between 5 months and 4 years. Results are highlighted in the table.
In accordance with previously published data, the study results further support promising outcomes of the application of NTG and HBOT to improve flap viability. Limitations include non-randomization of our treatment groups resulting in a retrospective evaluation of our protocol; and, the intrinsic heterogeneity of our patient population, previous surgical repairs, and scar tissues.
The proposed treatment of combining NTG and HBOT appears to result in the reversal of tissue hypoxia and improved wound healing. This preliminary report shows improved outcomes with less morbidity in a group of patients with multiple hypospadias surgical failures and it warrants further application in a larger number of patients.
Summary Table Single stage surgeries and complications. | |
Protocol (NTG + HBOT + local steroids) | No protocol (NTG + local steroids) |
45 patients Repair of recurrent glans dehiscence [13] Re-dehiscence 2/13 GTIP Urethroplasty [7] Urethral fistula 2/7 Urethral mobilization [6] No complications Repair of recurrent urethral fistula [10] Recurrent fistula 1/10 Recurrent chordee & stricture [5] and skin scarring [4] No complications | 33 patients Repair of recurrent glans dehiscence [11] Re-dehiscence 4/11 GTIP Urethroplasty [8] Glans Dehiscence & fistula 3/8 Urethral mobilization [9] Distal breakdown 2/9 Repair of recurrent urethral fistula [5] Recurrent fistula 2/5 |
Repeated surgeries for hypospadias result in varying degrees of scarring and hypervascularity of the tissues of the penile skin. The tissue ischemia may result in poor healing and the outcome is at best more scarring and at worst flap necrosis and breakdown of the repair. We set out to reduce the high postoperative complication rate in this group of patients and instituted a treatment protocol for patients who underwent multiple surgeries for hypospadias who often had compromised tissues. Our prior experience and the literature support that the local application of nitroglycerine (NTG) as a topical vasodilator enhances blood flow to skin flaps of children who underwent hypospadias repair [1] and post-mastectomy skin flaps [2]. A recent systematic review and meta-analysis of 6947 patients from 3 randomized controlled trials and 2 retrospective cohorts demonstrated NTG to be an ideal agent to increase the chance of flap survival in mastectomy flaps, with an excellent safety profile [3]. Hyperbaric oxygen therapy (HBOT) is a well-established mode of treatment and has several known cellular and biochemical benefits which promote wound healing, angiogenesis, and reversal of hypoxia. Herein we review the results of our strategy during the past 5.5 years of management of patients who presented with complex preoperative proximal hypospadias repairs using NTG ointment and HBOT. Each prior operation for hypospadias increases the odds of additional complications 1.5-fold with a complication rate of 40% with three or more re-operations [4]. We believe this rate is due to the poor vascularity of tissues. We hypothesized that methods to increase blood flow and promote wound healing, such as NTG and HBOT, would provide better outcomes in redoing hypospadias surgeries and reduce the complication rate. We also hypothesized that HBOT and NTG would reduce the complication rate compared to NTG alone.
Between May 2014 and November 2019, there were 82 patients (2-24 years old) who previously underwent multiple surgeries (3-9 operations, the average being 4.5 following primary repair and 5.5 total prior repairs) for hypospadias. All patients showed varying degrees of skin and subcutaneous scarring, which was noted either prior to or intraoperatively. All patients were recommended to undergo the protocol treatment which consisted of 2% NTG ointment applied at the conclusion of surgery, aiming at the enhancement of tissue perfusion by vasodilation (Fig. 1A-D). NTG was followed by 10 sessions of HBOT starting post-op day one. Each HBOT session included 90 min exposure to 100% Oxygen at 2 atm. 4-6 weeks later, patients applied local steroid cream to the wound (Betamethasone cream) for 3 months to prevent/reduce scarring and keloid formation. All patients were informed of the experimental and clinical evidence of the benefits of HBOT. They were asked to visit the HBO facility and were prepped by a board-certified physician about HBOT. Group, I consisted of all patients who completed the treatment protocol as described above. Group II patients received NTG and postoperative local steroid (same regimen as in Group I) but did not undergo HBOT for various reasons and served as the control group. These reasons included difficulty and failure to obtain insurance approval for HBOT, social issues, and residence too far from an HBOT facility. All of the patients’ insurance companies were contacted postoperatively, but approval was not granted for all patients. Those for whom insurance denied coverage for HBOT did not receive HBOT. Given that these were the reasons for patients not being able to receive HBOT, there is no selection bias by the surgeon. Patients were examined every 3 weeks for 3 office visits and were then examined every 3 months thereafter. The operative site was photographed at each visit.
The prior number of failed surgeries for hypospadias prior to inclusion in this study ranged from 3 to 9, with the average being 5.5. The initial surgical approach varied. The initial surgeries were performed by the senior author on 11/ 82 patients. However, 71 patients were self-referred, had previous surgeries elsewhere, and were frequently by different surgeons. Due to this, previous surgical details were not readily available. The position of the meatus was determined during the surgical repair and/or cystoscopy. The original site of the meatus was penoscrotal in 45 patients and mid or distal penile in 37 patients. The surgeries and complications for both groups of patients are demonstrated in Table 1. The operative procedures included single-stage repair in 45/49 patients. These included correction of recurrent glans dehiscence, recurrent urethral fistula (prior closures 4e5 attempts), and recurrent chordee with moderate or severe skin scarring, urethral mobilization, and grafted tabularized incised procedures (GTIP). 4 patients underwent staged repair, whereby the scarred tissues were excised and a urethral neo-plate created using a free graft of buccal mucosa which were subsequently tabularized 8e12 months postoperatively. In Group I, including patients who underwent single-stage and two-stage repairs, 44/49 (88.8%) had a successful outcome; namely a straight penis, a meatus at or near the tip of the glans penis, good forceful urine stream noted by parents, and/or the patient, and satisfactory cosmetic appearance noted by the parents and surgeon (Fig. 2). One patient developed a wound infection and the distal repair broke down. Another patient who had had five prior




Figure 1 a Hypospadias following 3 prior operations; b following urethral mobilization; c Nitroglycerine ointment applied to skin flap; d 3 months after 10 sessions of HBOT.
Table 1 Single stage surgeries and complications. | |
Protocol (NTG + HBOT + local steroids) | No protocol (NTG + local steroids) |
45 patients Repair of recurrent glans dehiscence [13] Re-dehiscence 2/13 GTIP Urethroplasty [7] Urethral fistula 2/7 Urethral mobilization [6] No complications Repair of recurrent urethral fistula [10] Recurrent fistula 1/10 Recurrent chordee & stricture [5] and skin scarring [4] No complications | 33 patients Repair of recurrent glans dehiscence [11] Re-dehiscence 4/11 GTIP Urethroplasty [8] Glans Dehiscence & fistula 3/8 Urethral mobilization [9] Distal breakdown 2/9 Repair of recurrent urethral fistula [5] Recurrent fistula 2/5 |
surgeries developed breakdown of the very distal repair, resulting in a low glandular subterminal meatus. However, the parents and surgeon felt that this was an acceptable result and the patient accepted the final outcome. Three patients developed urethral fistulas, which were subsequently repaired successfully. An example of the effectiveness of the dual therapy of NTG and HBOT is shown in Fig. 3a-e. This patient underwent 4 previous failed hypospadias repairs for proximal hypospadias. The photos demonstrate the surgical site at the end of the case, followed by severe venous congestion 4 h post-op. With NTG and HBOT, the surgical site had significant improvement at 7 days and 17 days postoperatively. The end result 6 weeks postoperatively shows a straight penis, the meatus at the tip of the glans, a good forceful urine stream, and good cosmesis. For all of the 4 patients who underwent staged repair, the oral mucosa grafts took well, healed satisfactorily, and subsequently tabularized successfully.
Another example of the dual therapy of NTG and HBOT is shown in Fig. 4aec. This is a 3-year-old patient who underwent 5 previous failed hypospadias repairs and intra-op was noted to have a penoscrotal meatus, along with significant scarring. A thigh graft was required for adequate coverage. After the application of NTG and undergoing HBOT, the end result 6 weeks postoperatively shows successful outcomes.
In Group II, 23 of 33 patients (69.6%) had successful results. 4 of these patients were lost to follow-up. 5 patients underwent additional surgery (two-stage repair of recurrent dehiscence in 4 patients, re-closure of urethral fistula in one patient) and 4/5 achieved successful outcomes. The fifth patient declined further surgery. The follow-up varied between 6 months and 3 years, and the median follow-up for the 2 groups was 14 months.
Following repeated attempts and surgeries for proximal hypospadias repair, the skin and tissues frequently become ischemic compared to the skin/tissues of a primary repair. The risk of complications increases to 40% with three or more redo hypospadias repairs [4], and we believe that the high complication rate is due to poor vascularity of tissues. Complications after primary repair requiring additional unplanned operations can be observed in up to 68% of patients with proximal hypospadias [5]. Generally, skin flap nonviability is believed to be related to the derangement of its microcirculation. Repair of hypospadias often necessitates the rotation of skin flaps, and in so doing the flap vascularity is subjected to some degree of trauma, which may induce vascular spasm. Vasospasm and blood sludging are probably the main adverse factors leading to ischemic necrosis of an otherwise well-designed, properly handled, and uninfected flap. In these cases, there is a short window of time when the ischemic tissues die and become necrotic and the use of NTG can be helpful.


Figure 2 a Pre-op. Prior 3 surgeries; b Post-op after grafted TIP, NTG, and HBOT.




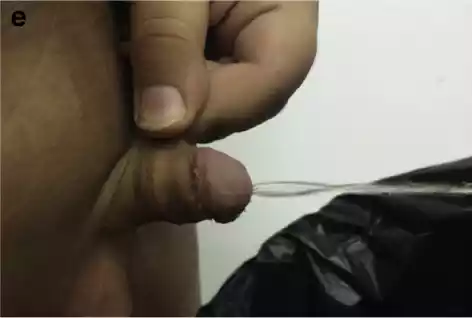
Figure 3 a Completed urethral mobilization of distal hypospadias: coronal meatus and skin scarring causing curvature (prior 4 surgeries); b Severe venous congestion noted 4 h after surgery; c One week after NTG and HBOT; d 17 days post op; E 6 weeks post-op.
Ischemic skin flaps and tissues occur in two forms, either due to arterial insufficiency with pale ischemic skin flaps, or inadequate venous drainage with a blue, more rigid flap with the rapid capillary refill. We believe that NTG increases blood flow due to vasodilation in the immediate postoperative period. Whereas, HBOT promotes angiogenesis, enhances fibroblast formation, and increases collagen formation during the subsequent healing phase in the postoperative days. We believe that the dual action reduced the complication rate and poor outcomes from multiple previous hypospadias repairs. The complication rate in the group who received NTG only was 30.4%, compared with the 11.2% of Group I who received both NTG and HBOT, suggesting some benefit of the HBOT.
NTG is a potent vasodilator with a large index of therapeutic safety. The first use and application of nitroglycerine to skin flaps in humans was in a study of penile skin in children undergoing circumcision and hypospadias repairs in 1986 [1]. Quantitative fluorescein studies were performed in a group of patients who underwent circumcision, and a prospective clinical trial of nitroglycerin was performed in 40 children undergoing hypospadias repair. Quantitative measurement of the fluorescence of NTG-treated skin flaps was performed, and the NTG-treated skin flaps had increased uptake of fluorescein. The conclusion was that NTG promotes increased net blood flow to skin flaps, and ultimately improves flap viability. Subsequently, a prospective study of NTG-treated skin flaps in children who underwent hypospadias repair compared with untreated flaps was carried out, which concluded that NTG improved skin flap survival. Since that study in 1986, we have applied 2% NTG to numerous skin flaps that appeared clinically ischemic (pale flap and/or blue flaps) with satisfactory results and salvage of the majority of these flaps [7]. Recently, a multi-institutional prospective randomized trial of NTG for post-mastectomy skin flaps was performed (2). NTG ointment or placebo was applied to the postmastectomy skin at the time of surgical dressing. The target sample size in the study was 400 patients, but the trial was stopped at the first interim analysis after 165 patients who were randomized (85 to the treatment group, and 80 to the placebo group). Mastectomy flap necrosis developed in 33.8% of patients who received a placebo and 15.3% of patients who received NTG ointment. Their conclusion was that NTG is an effective treatment for the prevention of mastectomy flap necrosis. One can therefore conclude from the studies that NTG reduces ischemia. The rationale for including the NTG in this protocol is to enhance the blood flow which is apt to increase tissue perfusion and oxygen supply to these sub-optimal skin flaps and tissues until HBOT, which was started the next day.
HBOT is a treatment modality in which a person breathes 100% oxygen while exposed to increased atmospheric pressure. Pressures applied while in the chamber were 1.4-2 atm absolute. During the HBOT children were able to watch videos or play games. Children and their caregivers
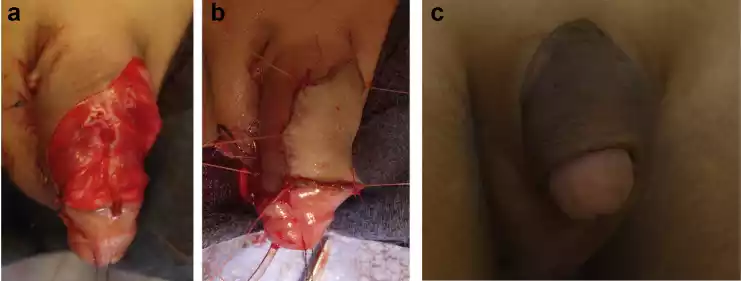
Figure 4 a 3-year-old male with 5 prior hypospadias operations. Intra-op, he was noted to have a penoscrotal meatus and significant scarring on both ventral and dorsal surfaces. This is the surgical site prior to placement of the graft, with a significant defect; b After placement of graft from the thigh, the patient had NTG applied and underwent HBOT starting post-op day one; c Surgical site 6 weeks postoperatively.
were given a thorough orientation to the HBOT chamber prior to starting treatment to help address any anxiety and to promote a successful treatment session. Generally, children tolerated the treatment well without adverse effects.
Wound healing is a complex process that is traditionally divided into inflammatory, proliferative, and remodeling phases. All processes occurring in these different phases including leukocyte activation, angiogenesis, collagen synthesis, and re-epithelialization, are all related to oxygen tension. The demand for oxygen in wound healing is the rationale for utilizing HBOT in compromised tissues where oxygen cannot sufficiently be delivered by the blood. The positive effect of HBOT on wound healing can be demonstrated more clearly in ischemic tissues. Using long-term intermittent HBOT, Kivisaari et al. [8] were able to enhance wound closure in experimental wounds with devascularized wound edges. They compared microvascular perfusion in normal and ischemic tissues (the latter was characterized by its inability to respond adequately to tissue injury). Despite the reduction in microvascular response to the tissue injury, HBOT was able to compensate for the failure of the vascular network, and these experiments showed that wound healing was similar in the HBOT group and in those with normal tissues.
The first experimental study of the role of HBOT in skin grafts of rats was carried out by Schulman and Krohn [9] in 1967. They reasoned that the skin grafts were relatively anoxic for the first few days after application of the graft, and therefore providing 100% oxygen under pressure would result in a more favorable oxygen environment at the surface of the wound. In the same year, Perrins [10] performed a prospective, randomized, blinded trial in which 24 patients who had free skin grafts received postoperative HBOT, while 24 other control patients did not. The HBOT was administered for 2 h on the evening of the operation and then thereafter twice per day for 3 days at 2 atmospheric pressure. There was an overall 29% improvement in graft survival in the HBOT group. Bowersox et al. [11] reviewed their experience with 65 patients who received HBOT for the threatened failure of skin flaps. 55% healed completely and 34% showed marked improvement. The experimental and clinical studies showed clearly the benefits of HBOT on graft take and ischemic flaps. Successful uses of HBOT for urinary tract diseases and abnormalities have also been reported for patients with radiation hemorrhagic cystitis [12].
We previously reported on our experience with 63 patients who had undergone multiple surgeries for hypospadias [13,14], and are included in this series. The repairs of the first 31 patients who received HBOT postoperatively were 90.6% successful with a notable decrease in postoperative edema. The current report confirmed the superiority of the proposed protocol and showed a lower complication rate in Group I (11.1%) than in the non-protocol Group II (33.3%).
We also used HBOT as an adjunctive treatment of hypospadias in six children who underwent two-stage repair using buccal mucosa grafts for salvaging the dehisced glans penis [15] and in four cases of urethroplasty for urethral strictures following hypospadias repair [16]. We believe that the HBOT contributed to the successful outcome in these cases, which had exhibited significant scarring. To our knowledge, the first publication on the use of HBOT for hypospadias was by Kara et al. [17] who reported on the beneficial effects of HBOT in adults who underwent tubed oral mucosal grafts.
A recent report described preemptively and not just postoperative use of HBOT. Seven pediatric “hypospadias cripples” who underwent a two-stage tabularized autograft surgical approach also underwent HBOT, and were noted to have good graft take with no graft contraction [18]. They concluded that preoperative HBOT can potentially reduce the expected high surgical failure secondary to graft contraction. However, 20 daily sessions of HBOT preoperatively Is impractical and is unlikely to be approved by the insurance carriers who only approve HBOT for failing grafts and/or flaps.
The side effects of HBOT are rare and usually treatments are well-tolerated. In unusual cases, patients can experience pulmonary barotrauma, pneumothorax, middle ear disturbances, and temporary myopia. In general, patients rarely require myringotomy tubes in order to tolerate getting to high pressure. However, none of our patients discontinued the therapy due to these side effects. In Group II many patients were unable to obtain insurance approval within a reasonable time period and were restricted due to the financial impact of therapy. Some were skeptical and some resided too far from the HBOT facility.
We instituted the postoperative use of topical betamethasone to avoid scar and keloid formation. Corticosteroids have been demonstrated to interrupt the inflammatory process, reduce fibroblast and keratinocyte proliferation, and have antimitotic activity [19,20]. The topical steroids have been shown to prevent or decrease scarring and/or keloid formation [21,22].
One limitation of this study is that although it started as a prospective study, the non-randomization of our treatment groups resulted in a retrospective evaluation of our protocol and using the non-treatment group as a control. However, it is conceivable that patient and family-member compliance with the treatment protocol may reflect a family that is more diligent and otherwise more likely to adhere to postoperative care recommendations and restrictions of their child’s activity following surgery. Furthermore, another limitation of the study is the intrinsic heterogeneity of our patient population and surgical repairs. Given our study design, it is not possible to know the severity of the original hypospadias in all patients, nor is it possible to know the type of prior surgeries. Within each of the two groups, there is heterogeneity with respect to prior scar tissue, vascularity, and aesthetic quality and no two cases are the same; however, these variations exist in all patients with prior failed hypospadias repairs and reflect the nature of the reports on re-do hypospadias repairs. They were comparable in that they all endured at least 4 operations, and therefore had poorly vascularized skin and tissues, and exhibited excessive scarring. Additionally, it may be argued that since both HBOT and NTG were given to patients, it may be difficult to separate the effect of one from the other. Another limitation of this study is the lack of statistical analysis. Furthermore, follow-up ranged from 5 months to 4 years, but ideally, all patients would be followed for at least 2 years post-repair.
The quality of the tissues and skin is suboptimal following multiple hypospadias repairs. The tissues and skin are scarred and ischemic. Flap nonviability is believed to be related to the derangement of its microcirculation. NTG is a safe and potent vasodilator, and its application at the conclusion of surgery can improve the blood flow to the compromised tissues of patients who have had repeated hypospadias surgeries. Its benefits in reducing postmastectomy flaps by nearly 50% have been described extensively and in prospective randomized trials. Additionally, there is strong experimental and clinical evidence to support the contribution of HBOT to wound healing in compromised flaps and grafts, which are by nature ischemic. Our study suggests that HBOT is beneficial in this group. The proposed treatment modality of HBOT and NTG appears to result in the reversal of tissue hypoxia and improved wound healing by enhancing tissue circulation, improving vascularization, and promoting angiogenesis. This preliminary report should prompt further studies and add to the surgical armamentarium for repeat hypospadias repairs for patients who had endured multiple surgical procedures. Currently, we apply NTG to any ischemic flap and counsel patients about the benefits of HBOT to all patients who are planning repeat surgeries for hypospadias repairs.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
None declared.
A Department of Surgery, Division of Urology, Rutgers – New Jersey Medical School, 140 Bergen Street, G1680, Newark, NJ, 07103, USA
b Hyperbaric Medical Solutions, 160 E 32nd St #101, New York, NY 10016, USA
c New York Presbyterian-Weill Cornell Medical Center, 525 E 68th St, New York, NY, 10065, USA
* Correspondence to: Chrystal Chang. [email protected] (C. Chang)
Keywords
Redo hypospadias; Hyperbaric oxygen; Nitroglycerine; Skin flap ischemia
Abbreviations
NTG, Nitroglycerine; HBOT, Hyperbaric oxygen therapy
Received 9 April 2020 Revised 15 July 2020 Accepted 23 July 2020 Available online 31 July 2020
We have locations in the Arlington, Flower Mound, Keller, Lewisville, Stone Oak, Kingwood, Frisco, Pearland, Argyle Texas. Contact one of our offices to make an appointment to begin healing today.
WOUND CARE AND HYPERBARIC OXYGEN THERAPY
Located in The Dallas-Fort WORTH, Houston and San Antonio Areas of Texas