Yeji Ahn1 , Young Joon Seo1,2 , Young Sub Lee1,2
1 Research Institute of Hearing Enhancement, Wonju College of Medicine, Yonsei University, Wonju, South Korea 2 Department of Otorhinolaryngology, Wonju College of Medicine, Yonsei University, Wonju, South Korea
ORCID IDs of the authors: Y.J.S. 0000-0003-1169-0441; Y.S.L. 0000-0002-4423-8905
Cite this article as: Ahn Y, Joon Seo Y, Sub Lee Y. The effectiveness of hyperbaric oxygen therapy in severe idiopathic sudden sensorineural hearing loss. J Int Adv Otol. 2021;17(3):215-220.
OBJECTIVE: To evaluate the effect of combined hyperbaric oxygen therapy (HBOT) and steroid therapy in severe idiopathic sudden sensorineural hearing loss (ISSNHL).
METHODS: Between January 2010 and July 2017, we evaluated 218 patients with ISSNHL and divided them into 2 groups: those with hearing loss greater than 80 dB and those with hearing loss of 60-79 dB. Each group was further divided into 3 groups according to the treatment method: oral steroids alone (PO), PO+intratympanic injection (IT), and PO+IT+HBOT. The treatment effect was evaluated for improvement in hearing thresholds at mid-term (3 weeks later) and final term (2 months later).
RESULTS: When comparing the 3 treatment groups within the group that had a hearing loss greater than 80 dB, no differences were observed in the gaps in hearing thresholds and in the duration of improvement (P = .0764 and .2938, respectively). However, in the group with 60-79 dB hearing loss, the gaps in hearing thresholds at mid-term were 27.50 dB in the PO group, 38.13 dB in the PO+IT group, and 51.25 dB in the PO+IT+HBOT group. The treatment was more effective and faster in the initial period in the PO+IT+HBOT group than in the other groups. In addition, the results of frequency analysis showed the greatest treatment efficacy at low frequencies of hearing. CONCLUSION: Patients with ISSNHL above 80 dB are less likely to recover hearing even after PO+IT+HBOT. However, this treatment initially accelerates recovery in patients with hearing loss below 80 dB. Therefore, the appropriate indication for HBOT benefits in patients with severe or profound ISSNHL should be reviewed.
KEYWORDS: Hyperbaric oxygen therapy, idiopathic sudden sensorineural hearing loss, steroid, intratympanic injection
Idiopathic sudden sensorineural hearing loss (ISSNHL) is defined as a sudden hearing loss that has no known cause, and it occurs in 3 days or more with 30 dB of sensorineural hearing loss at 3 or more consecutive frequencies on pure-tone audiometry (PTA).1 Initially, patients may complain of tinnitus or ear fullness, and accompanying dizziness may occur in approximately 20-60% of patients; however, these symptoms are not severe and usually disappear within a few days.2,3
Therapies for unexplained sudden hearing loss are unclear. Therefore, anti-inflammatory drugs, blood circulation improvement, vasodilators, antiviral drugs, and diuretics may be used.4,5 Among them, steroids are the only ones recognized for their effectiveness in sudden hearing loss.6 They may be used in combination with one or more agents, such as acyclovir, dextran, Ginkgo biloba, nifedipine, magnesium, vitamins (B, E, and C), pentoxifylline, carbogen, heparin, or histamine, as well as other therapies, such as stellate ganglion block or hyperbaric oxygen therapy (HBOT).7,8 Many clinical practice guidelines have recommended HBOT as a combination treatment for ISSNHL.9-11 Although the exact mechanisms underlying the effect of HBOT on ISSNHL are unclear, HBOT can enhance the positive effects of steroids in reducing vascular permeability, edema, and inflammatory responses7.
In accordance with the International Organization for Standardization in 1964, the degrees of hearing loss are classified as follows: less than 25 dB HL (normal), 26-40 dB HL (mild hearing loss), 41-55 dB HL (moderate hearing loss), 56-70 dB HL (moderate to a severe hearing loss), 71-90 dB HL (severe hearing loss), and greater than 91 dB HL (profound hearing loss).12 The more severe the hearing loss on an initial test or the more the hearing loss over the whole frequencies of the test, the poorer the prognosis of recovery for ISSNHL.13,14 Children and elderly people have a relatively low recovery rate, and patients with long-term ISSNHL may show less recovery.15
In this study, we investigated the necessity of routine application of combined steroid therapy and HBOT for severe or profound ISSNHL and attempted to define the indications of hearing thresholds on PTA for HBOT.
We recruited 218 patients treated retrospectively for ISSNHL between January 2010 and July 2017. The patients were divided into 2 groups according to the insurance policy standard PTA of 80 dB for HBOT. Among the patients with greater than 80 dB hearing loss, 47 were treated using oral steroids (PO) alone, 62 were treated using PO and intratympanic (IT) injection of dexamethasone (PO+IT), and 37 were treated using PO, IT injection of dexamethasone, and HBOT (PO+IT+HBOT). Among the patients with 60-79 dB hearing loss, 27 were treated using PO alone, 18 were treated using PO+IT, and 16 were treated using PO+IT+HBOT.
HBOT was performed 10-20 times for 100 min/day using 100% pure O2 for ventilation at 2.0 atmosphere absolute, according to the protocol of our hospital. Oral steroid therapy was started at 5 days, with a high dose of methylon (48 mg # 2), and discontinued after tapering over 5 days. IT dexamethasone (5 mg/mL) injection into the inner ear through the tympanic membrane was performed under a surgical microscope by an otolaryngologist. The head was turned to the opposite side in the supine position, and the position was maintained for 30 min to ensure the medicine was not discharged through the ear or swallowed. Three injections were performed every other day during the hospitalization period.
Pure-tone thresholds were obtained for air conduction at 250 Hz, 500 Hz, 1 kHz, 2 kHz, 4 kHz, and 8 kHz and for bone conduction at 250 Hz, 500 Hz, 1 kHz, 2 kHz, and 4 kHz. Audiologic data were reported according to the methods recommended by the Hearing and Equilibrium Committee of the American Academy of Otolaryngology-Head and Neck Surgery. Patients were evaluated according to the recovery observed during the 2-month follow-up period. Following our protocol of ISSNHL treatment, PTA was performed on the day of admission, the 5th hospitalization day (day of discharge), the 1st clinical follow-up date (2 weeks after discharge), and the 2nd clinical follow-up date (1 month after discharge). PTA was performed on the basis of the patient’s responses to treatment, and the results were classified according to Siegel’s criteria[5]. The patients were then divided into 2 groups as follows: a recovery group (complete + partial + slight recovery) if they showed a 15-dB improvement in hearing, and a non-recovery group if they showed no improvement. We considered the degree of recovery as the gap between the initial and final PTA and measured it. The thresholds of follow-up PTA were defined as mid-term PTA at about 3 weeks after treatment. The first recovery time indicated the time of initial hearing recovery according to Siegel’s criteria. The final recovery time was noted as the duration of the final follow-up.
A power analysis was performed to determine if the proposed sample size would be adequate (effect size = 0.08; α-risk = 0.05; sample size=16). Continuous variables were summarized as mean ± standard deviation. General characteristics between the groups were evaluated using analysis of variance (ANOVA) and a Chi-squared test. Pure tones between the groups were evaluated using ANOVA and the Kruskal– Wallis test. Box and whisker plots were used to evaluate pure-tone distributions, and recovery duration was analyzed using the Kaplan– Meier method. SAS v9.4 (SAS Institute, Cary, NC) was used for statistical analysis, and differences were considered significant at P < .05.
The Effectiveness of HBOT in Patients With Severe to Profound ISSNHL (>80 dB)
Table 1 shows the results of the general characterization of variables, such as age, sex, diabetes history, hypertension history, body mass index, hemoglobin level, and white blood cell count, in the PO, PO+IT, and PO+IT+HBOT groups of patients with greater than 80 dB hearing loss. The neutrophil counts were 6.75 ± 4.04, 5.64 ± 2.81, and 7.41 ± 3.51 in patients who received PO, PO+IT, and PO+IT+HBOT (P = .037), respectively. Significant differences were also observed in the neutrophil/lymphocyte ratios (NLRs), with corresponding values of 5.44 ± 5.21, 4.19 ± 2.94, and 6.88 ± 5.60 (P = .017), respectively.
Table 1. General Characteristics of the 3 Groups of Patients With Greater Than 80 dB Hearing Loss
PO (n = 47) | PO+IT (n = 62) | PO+IT+HBOT (n = 37) | P | |
Age (years) | 56.85 ± 16.67 | 52.18 ± 15.04 | 53.32 ± 17.36 | .3179 |
Sex (M, %) | 20 (42.6) | 30 (48.4) | 17 (45.9) | .8326 |
DM Hx (%) | 10 (21.3) | 14 (22.6) | 7 (18.9) | .9113 |
HTN Hx (%) | 19 (40.4) | 24 (38.7) | 12 (32.4) | .7361 |
BMI (kg/m²) | 23.71 ± 3.73 | 24.85 ± 3.82 | 25.37 ± 3.41 | .1379 |
WBC | 9.1 ± 3.86 | 15.99 ± 63.83 | 9.49 ± 3.27 | .0349* |
Neutrophil | 6.75 ± 4.04 | 5.64 ± 2.81 | 7.41 ± 3.51 | .0370* |
Lymphocyte | 1.67 ± 0.75 | 1.7±0.83 | 1.50 ± 0.73 | .4179 |
Monocyte | 0.4 ± 0.22 | 0.31 ± 0.13 | 0.35 ± 0.18 | .0595 |
PLT | 253.28 ± 68.54 | 237.16 ± 52.39 | 236.05 ± 53.85 | .2812 |
NLR | 5.44 ± 5.21 | 4.19 ± 2.94 | 6.88 ± 5.60 | .0173* |
PLR | 183.67 ± 90.75 | 168.58 ± 81.34 | 203.88 ± 114.45 | .1951 |
The values are mean ± standard deviation or frequency (n), *P < .05. PO = oral steroid group; PO+IT = oral steroid and intratympanic injection group; PO+IT+HBOT = oral steroid, intratympanic injection, and hyperbaric oxygen therapy group; DM Hx = diabetes mellitus history; HTN Hx = hypertension history.
BMI, body mass index; WBC, white blood cell; PLT, platelet; NLR, neutrophil/lymphocyte ratio; PLR, platelet/lymphocyte ratio.
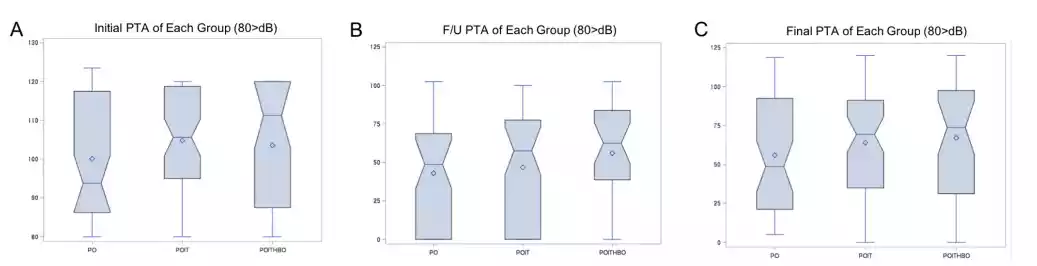
Figure 1. Comparisons of hearing thresholds in patients with severe to profound idiopathic sudden sensorineural hearing loss (ISSNHL) having greater than 80 dB hearing loss according to the 3 different treatments. (A) Initial pure-tone audiometry (PTA), (B) follow-up PTA at mid-term (3 weeks after treatment), and (C) final PTA at the final term (2 months after treatment). PO = oral steroid alone; IT = intratympanic injection; HBOT = hyperbaric oxygen therapy.
The PTA thresholds of the 3 groups with greater than 80 dB hearing loss were compared during the follow-up periods: initial PTA, follow-up PTA, and final PTA (Figure 1). The median initial threshold of hearing loss was higher in the HBOT group than in the other groups, with a median of 93.75 dB in the PO group, 105.63 dB in the PO+IT group, and 113.75 dB in the HBOT group (P = .239). The final PTA among the groups also showed no differences (P = .074). The gap between the initial and final PTA was 44.12 ± 28.19 dB in the PO group, 40.77 ± 31.55 dB in the PO+IT group, and 27.7 ± 26.74 dB in the HBOT group, indicating a low value of hearing recovery in the HBOT group (P = .076). The statistical analysis between the groups for each frequency of PTA did not yield significant results. Analysis of the duration to recovery by using Kaplan–-Meier curves in the patient groups with greater than 80 dB hearing loss showed no significant differences between the treatment groups, and the P value of the log-rank test was .0582 (Figure 2).
The Effectiveness of HBOT in Patients With Severe ISSNHL (60-79 dB)
Table 2 shows the results of the general characterization of the PO, PO+IT, and PO+IT+HBOT groups with initial PTA thresholds of
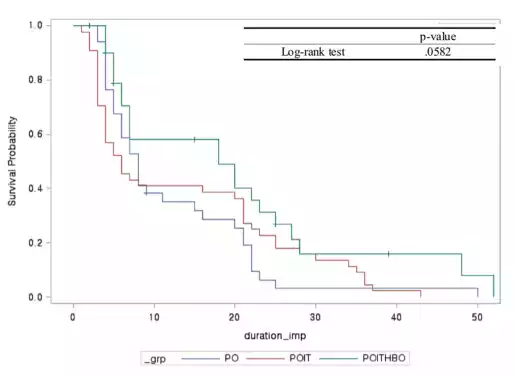
Figure 2. Recovery duration of the 3 groups of patients with greater than 80 dB hearing loss. PO = oral steroid alone; IT = intratympanic injection; HBOT = hyperbaric oxygen therapy.
60-79 dB. Although the initial PTA thresholds were significantly different among the groups (73.75 dB, 67.50 dB, and 73.75 dB, respectively; P = .047; Figure 3), the average gaps between the initial and follow-up PTA were 28.75 dB in the PO group, 47.50 dB in the PO+IT group, and 68.13 dB in the PO+IT+HBOT group (Figure 4A), with a significant P value of .041. However, the gaps between the initial and final PTA did not show significant differences between the groups (P = .097; Figure 4B).
The comparison of the difference in PTA by frequency in the patient groups with 60-79 dB hearing loss showed that the effect on recovery was high in the HBOT group, especially at low frequencies at the follow-up period (about 3 weeks); P value = .005 at 250 Hz, .0004 at 500 Hz, .001 at 1000 Hz, .003 at 2000 Hz, .035 at 4000 Hz, and .003 at 8000 Hz (Figure 5). Taken together, these results suggest that in the treatment of patients with ISSNHL with 60-79 dB hearing loss, HBOT improves the outcomes more quickly than the other treatments at the initial 3-week follow-up, primarily improving low-frequency hearing.
In 1970, many researchers considered circulatory impairment as the main cause of sudden hearing loss and started using HBOT for its treatment.9-11,16 According to the 2019 American Academy of Otolaryngology-Head and Neck Surgery Guidelines (updated) for the Treatment of Hearing Loss, steroid therapy and HBOT are the first options; moreover, the guidelines recommend that treatment be determined in consideration of clinician judgment and patient preference7.
Since September 1, 2016, the National Health Insurance Corporation of Korea started granting insurance benefits for HBOT when it was performed once within 60 to 120 min in patients with ISSNHL having an initial hearing threshold of 80 dB or more. In Korea, data analysis for 2 years from 2012 to 2013 showed that HBOT was used more commonly for treating carbon monoxide poisoning, wound defects after skin transplantation, air embolism, necrotic soft-tissue infections, thermal burns, diabetic foot, and decompression sickness rather than for treating ISSNHL. We thought the reason why HBOT was not well used in Korea was that the insurance coverage was limited to patients with severe to profound ISSNHL. Therefore, this study was conducted to confirm the effectiveness of HBOT in patients with severe to profound ISSNHL and to propose indications for the hearing thresholds in the treatment of ISSNHL.
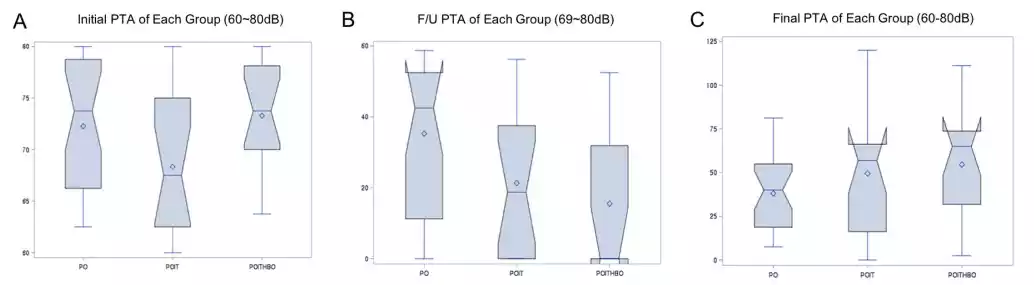
Figure 3. Comparisons of hearing thresholds in patients with severe to profound idiopathic sudden sensorineural hearing loss (ISSNHL) having 60-79 dB hearing loss according to the 3 different treatments. (A) Initial pure-tone audiometry (PTA), (B) follow-up PTA at mid-term (3 weeks after treatment), and (C) final PTA at the final term (2 months after treatment). PO = oral steroid alone; IT = intratympanic injection; HBOT = hyperbaric oxygen therapy.
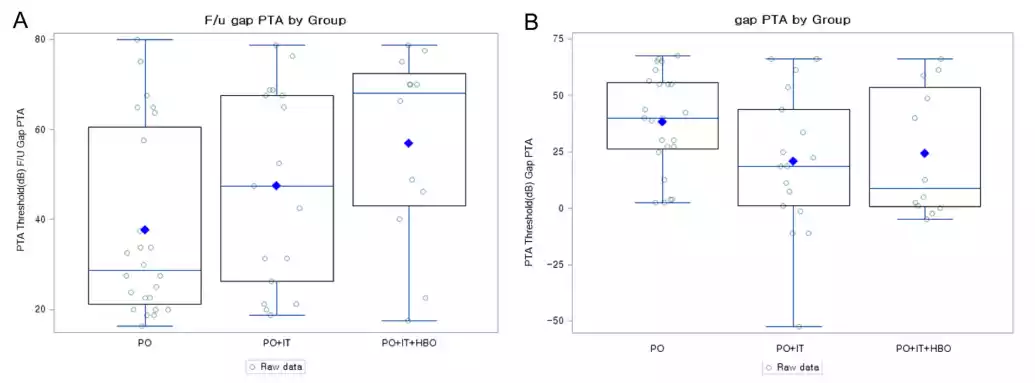
Figure 4. The gap in hearing thresholds in the 3 groups. (A) The gap at the mid-term follow-up: 28.75 dB in the oral steroid alone (PO) group, 47.50 dB in the oral steroid and intratympanic injection (PO+IT) group, and 68.13 dB in the oral steroid, intratympanic injection, and hyperbaric oxygen therapy (PO+IT+HBOT) group (P = .041). (B) The gap at the final term (no differences among the groups).
In the literature, 41-61% of patients recovered from acute hearing loss by using steroids, the most commonly used therapeutic agent for ISSNHL.17 Currently, most combinations of drugs with steroids are used in patients with ISSNHL. The rationale for the application of HBOT to sudden hearing loss is that the cause of vascular problems (viruses, autoimmunity, etc.) eventually results in cochlear injury owing to hypoxia. The accumulation of carbon dioxide causes anaerobic glycolysis, oxidation, tissue edema, and reduced blood flow.18 Many studies have shown that HBOT has an additional therapeutic effect when used in combination with steroid therapy. This study used a combination of a systemic steroid, IT injection, and HBOT in patients with ISSNHL. As shown in Table 1, the NLR values of the 3 groups showed statistically significant differences. Previous studies confirmed that the recurrence and prognosis of sudden hearing loss could be predicted through the NLR and platelet/lymphocyte ratio.19 In ISSNHL, systemic steroids and IT injections are more effective than systemic steroids alone.20 Topuz et al. reported that HBOT was better for patients under 50 years of age, and that hearing recovery was better at lower frequencies than at higher frequencies.21
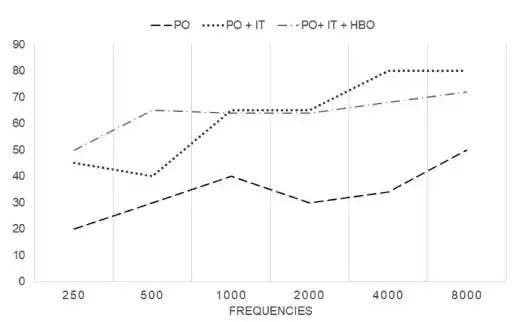
Figure 5. Pure-tone audiometry (PTA) differences according to frequencies (Hz) among the 3 groups of patients with less than 80 dB (60-79 dB) hearing loss.
Our study comprised 3 groups in which additional treatments were provided together with oral steroids. In patients with greater than 80 dB hearing loss after the treatments, the final hearing thresholds were the highest in the HBOT group, and the difference in the gap between the initial and final PTA for hearing recovery was the least, albeit not statistically significant. HBOT resulted in a significantly faster improvement in hearing recovery at the initial recovery periods in the severe ISSNHL group (60-79 dB of initial PTA) than in the control group, with significant differences, especially at low frequencies. These results may suggest that HBOT is ineffective in ISSNHL with greater than 80 dB hearing loss. Another study showed that the higher the initial hearing loss, the lower the probability of complete recovery.11 In the mild hearing loss, the recovery rate reached 83%, but in severe hearing loss, the recovery rate was only 22%. Steroid administration was also ineffective in patients with ISSNHL having greater than 90 dB hearing loss. Wilson et al. reported that 61% of patients with hearing loss showed improvements with oral steroids, whereas patients with greater than 90 dB of hearing loss did not show any improvement.22 In patients with ISSNHL having greater than 80 dB hearing loss, irreversible changes may possibly occur in the hair cells of the cochlea. Although HBOT restores hypoxic damage, it is ineffective in patients with irreversible hearing loss above 80 dB and only initially accelerates recovery in patients with a possibility of reversible hearing loss below 80 dB.
Table 2. General Characteristics of the 3 Groups of Patients with 60-79 dB Hearing Loss
PO (n = 27) | PO+IT (n = 18) | PO+IT+HBOT (n = 16) | P | |
Age (years) | 52 (18-80) | 50 (17-78) | 55 (35-78) | .4575 |
Sex (M, %) | 13 (48.15) | 10 (55.56) | 4 (25.00) | .1736 |
DM Hx (%) | 3 (11.11) | 8 (44.44) | 4 (25.00) | .0390 |
HTN Hx (%) | 5 (18.52) | 8 (44.44) | 6 (37.50) | .1501 |
BMI (kg/m²) | 23.6 (18.66-32.9) | 24.94 (18.5-37.2) | 23.82 (20.61-27.6) | .6108 |
WBC | 8.8 (0.69-16.76) | 7.3 (4.57-16.09) | 9.87 (5.15-14.26) | .4126 |
Neutrophil | 6.33 (1.99-15.95) | 4.31 (1.86-13.76) | 8.52 (2.65-12.4) | .1279 |
Lymphocyte | 2.15 (0.49-4.18) | 2.01 (1.42-3.13) | 1.37 (0.66-2.65) | .0443* |
Monocyte | 0.43 (0.09-0.98) | 0.32 (0.14-1.33) | 0.28 (0.14-0.75) | .5186 |
PLT | 258 (156-397) | 269.5 (196-440) | 247 (0.02-341) | .4049 |
NLR | 2.44 (0.97-27.03) | 2.39 (0.89-7.64) | 6.74 (1.34-14.35) | .0108* |
PLR | 111.9 (55.25-645.76) | 139.59 (85.61-202.76) | 137.67 (0.02-405.88) | .3050 |
The values are mean ± standard deviation or frequency (n), *P < .05.
PO = oral steroid group; PO+IT = oral steroid and intratympanic injection group; PO+IT+HBOT = oral steroid, intratympanic injection, and hyperbaric oxygen therapy group; DM
Hx = diabetes mellitus history; HTN Hx = hypertension history.
BMI, body mass index; WBC, white blood cell; PLT, platelet; NLR, neutrophil/lymphocyte ratio; PLR, platelet/lymphocyte ratio.
HBOT definitely would be an option for treatment combined with steroid medications for ISSNHL. But the indications for the HBOT should be developed in further studies. In this study, we revealed that severe hearing loss in the irreversible stage could not be recovered by HBOT according to our regimen. The hair cells of the cochlea in the reversible stage could be rescued effectively by HBOT. This finding would be important evidence to widen the indications of treatments in patients with ISSNHL.
Ethics Committee Approval: All subjects provided written consent on their treatments with HBOT. The study was conducted according to the Helsinki Declaration guidelines and received approval from the Yonsei Wonju University of Medicine Review Board(IRB#CR317065).
Informed Consent: All patients interested in participating in this prospective trial who met the inclusion criteria signed informed consent.
Peer Review: Externally peer-reviewed.
Author Contributions: Concept – Y.J.S.; Design – Y.J.S.; Supervision – Y.J.S; Resource – Y.J.A and Y.S.L.; Materials – Y.J.A and Y.S.L.; Data Collection and/or Processing – Y.S.L.; Analysis and/or Interpretation – Y.J.S and Y.S.L.; Literature Search – Y.J.A and Y.S.L.; Writing – Y.J.A, Y.J.S., and Y.S.L.; Critical Reviews – Y.J.S.
Acknowledgments: This work was supported by the Technology Innovation Program(20010587, Development and Dissemination on National Standard Reference Data) funded By the Ministry of Trade, Industry & Energy(MOTIE, Korea) and by National Information Society Agency(NIA) funded by the Ministry of Science, ICT.
Conflict of Interest: The authors have no conflict of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
We have locations in Arlington, Flower Mound, Keller, Lewisville, Stone Oak, Kingwood, Frisco, Pearland, Argyle Texas. Contact one of our offices to make an appointment to begin healing today.
WOUND CARE AND HYPERBARIC OXYGEN THERAPY
Located in The Dallas-Fort WORTH, Houston and San Antonio Areas of Texas